The US could be on the cusp of a seismic shift in childhood immunization policy. A federal advisory panel, now chaired by Kirk Milhoan and appointed under Health Secretary Robert F. Kennedy Jr., is set to vote on whether to end the decades-old recommendation that all newborns receive the hepatitis B vaccine within 24 hours of birth. The ramifications go far beyond one shot—this debate touches the foundation of public health in America.
Let’s cut through the noise, analyze the broader implications, and spotlight what most people overlook in this heated controversy.
Why This Matters
- Public Health Precedent: The hepatitis B vaccine for newborns has been a cornerstone of US immunization policy since 1991, credited with a 99% decline in acute hepatitis B among children and young adults between 1990 and 2019 (study).
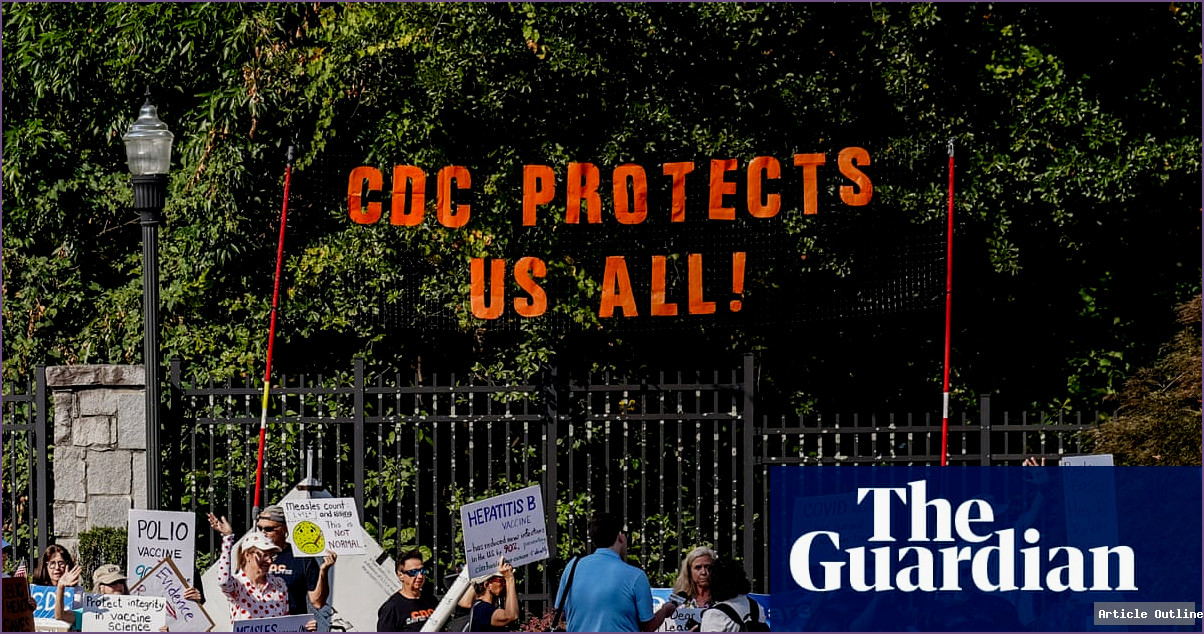
- Broader Immunization Impact: Reversing this recommendation could trigger a domino effect, emboldening efforts to roll back other childhood vaccines and upend trust in science-backed health policies.
- Political & Ideological Shift: This isn’t just a scientific debate—it’s a reflection of new political leadership’s skepticism toward established medical consensus. The CDC has already changed its public statements on vaccine safety under Kennedy’s direction.
What Most People Miss
- Delayed Vaccines = Increased Risk: Hepatitis B is often transmitted from mother to child at birth, even if the mother is not known to be infected. Delaying the vaccine leaves a critical vulnerability in the first months of life, especially since many infections are asymptomatic in mothers.
- The Data Speaks: The overwhelming decline in pediatric hepatitis B cases—99%—is a direct result of universal newborn vaccination. Countries that have delayed or skipped this vaccine have seen persistent or resurgent infections.
- Focus on Allergies and Autoimmune Diseases: The panel claims it is exploring links between vaccines and the rise in allergies/autoimmune disorders, but robust studies consistently find no causal link between standard vaccines and these chronic conditions.
- Aluminum Adjuvant Concerns: Much is made of aluminum salts in vaccines, yet the actual exposure is minuscule compared to everyday sources (food, water, environment). Regulatory bodies worldwide maintain these levels are well within safe limits, especially given the benefits of vaccination.
Key Takeaways
- Science vs. Politics: The current panel’s makeup is less about fresh science and more about ideology. This should raise alarms for anyone who values evidence-based policy.
- Real-World Consequences: Recent outbreaks in the US—measles deaths in Texas, pertussis deaths in Kentucky—have been traced to declining vaccination rates. History is repeating itself in real time.
- Global Comparisons: Countries with lower vaccine coverage, or with delayed hepatitis B schedules, report higher rates of childhood hepatitis B, leading to lifelong health complications and increased liver cancer risk.
Expert Commentary
William Matthew London, editor of Quackwatch, expressed blunt skepticism: “The CDC…is no longer a trustworthy source of health information.”
Meanwhile, public health professionals warn that dismantling proven vaccine schedules is a “reckless disregard for science and the truth.”
Timeline: From Recommendation to Reversal?
- 1991: Hepatitis B vaccine recommended for all US newborns
- 1990–2019: Acute hepatitis B declines by 99% in children and young adults
- 2025: New Kennedy-appointed panel considers scrapping the recommendation
- This week: Vote expected on whether to delay or drop the universal newborn dose
The Bottom Line
This is more than a technical policy tweak. It’s a high-stakes test of whether public health in America will continue to be steered by rigorous science—or by ideology and misinformation. The hepatitis B vaccine for infants isn’t just about hepatitis B; it’s a bellwether for the future of vaccination and public trust in health institutions.